Research News: Improving outcomes for patients with sciatica
By Crystal Mackay MA’05
Patients diagnosed with sciatica experience shooting pain that radiates from the lower back through the hips and down the leg. It’s a condition that can affect quality of life especially for the 10 per cent who don’t get better on their own. To improve outcomes for these chronic patients, Dr. Christopher Bailey and team demonstrated through a randomized controlled trial that undergoing spine surgery improved their experience of pain versus non-operative treatment.
The study, “Surgery versus Conservative Care for Persistent Sciatica Lasting 4 to 12 Months,” was recently published in the New England Journal of Medicine.
“There have been a number of studies which show that the longer you have the symptoms, the less likely you’ll respond to treatment well,” said Dr. Bailey, an Associate Professor in the Department of Surgery at Schulich Medicine & Dentistry. “No one has specifically compared operative and non-operative care for these chronic patients. We are the first to make that comparison.”
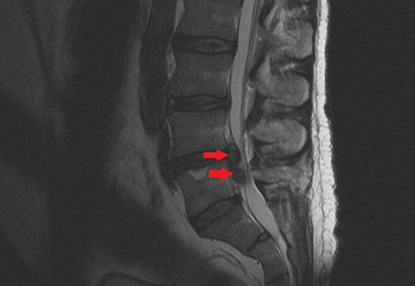 Sciatica is caused by lower back disc herniation, where the cushions between the vertebrae herniate and press up against the nerves that run in the spinal canal. The prognosis is generally good, and 90 per cent of patients will get better within a few months. For the 10 per cent of patients who experience pain longer than four months, it wasn’t well known whether they would have better outcomes through surgery to remove the fragmented disc that is pressing on the nerve, or through a combination of physiotherapy, medication, injections, and exercise.
Sciatica is caused by lower back disc herniation, where the cushions between the vertebrae herniate and press up against the nerves that run in the spinal canal. The prognosis is generally good, and 90 per cent of patients will get better within a few months. For the 10 per cent of patients who experience pain longer than four months, it wasn’t well known whether they would have better outcomes through surgery to remove the fragmented disc that is pressing on the nerve, or through a combination of physiotherapy, medication, injections, and exercise.
The study authors recruited 128 patients with persistent sciatica who were assigned to either receive surgery or non-surgical care, and evaluated their leg pain intensity after six months. At baseline, the mean score for leg-pain intensity was 7.7 in the surgical group and 8.0 in the nonsurgical group. The leg-pain intensity score at 6 months was 2.8 in the surgical group and 5.2 in the nonsurgical group, showing a substantial improvement for the group that underwent surgery.
“This surgery for sciatica is one of the top three most common operations we perform as spinal surgeons in Canada,” Dr. Bailey said. “The people who need surgery are those for whom the pain is so significant that it compromises their function and quality of life. Those are the patients who are included in this study.”
The study authors were able to take advantage of the wait times for surgery in the Canadian system to accurately randomize the groups, by referring patients waiting for surgery to receive the non-operative treatment during the waiting period. The patients in the non-surgical group did eventually receive surgery so no treatment was withheld.
“We were able to design a study which had two discrete treatment groups for comparison at the primary outcome which was six months,” he said. “The patients that were referred to us normally would wait some time to see a surgeon, so we recruited them immediately upon referral into the study and they were referred to see the study spine specialist. The spine specialist would either provide them with the optimal non-operative care or surgery if they qualified. So, in that way, treatment was never withheld, they were actually given care that they would not have been receiving if they were still waiting to see a surgeon outside of the study.”









