World AIDS Day: Decoding HIV’s stealth strategy
 Stephen Barr, PhD, and his research team have made significant strides in understanding the intricate mechanisms by which HIV interacts with and evades the human immune system. (National Institute of Allergy and Infectious Diseases/Flickr)
Stephen Barr, PhD, and his research team have made significant strides in understanding the intricate mechanisms by which HIV interacts with and evades the human immune system. (National Institute of Allergy and Infectious Diseases/Flickr)
Prabhjot Sohal
It was learning about the vast historical impacts of the Spanish Flu and the Black Plague in high school that sparked virologist Stephen Barr's interest in infectious diseases.
“I was shocked at how seemingly simple pathogens could decimate the human population,” said Barr, PhD, associate professor of molecular virology at Schulich School of Medicine & Dentistry.
However, it was HIV and its ability to trick and evade the human body’s immune system that captured and shaped Barr’s research.
“HIV is a virus encoding only about 15 proteins, yet it can wreak havoc in human populations,” he said.
Over the past decade, the Barr Lab has made significant strides in understanding the intricate mechanisms by which HIV interacts with and evades the human immune system.
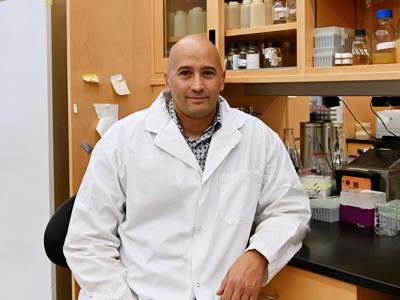 Stephen Barr, PhD, Associate Professor, Microbiology and Immunology (Prabhjot Sohal/Schulich Medicine & Dentistry)
Stephen Barr, PhD, Associate Professor, Microbiology and Immunology (Prabhjot Sohal/Schulich Medicine & Dentistry)
A pivotal achievement of the lab is the discovery of protein named HERC5, which plays a vital role in the body's interferon response – the first line of defense against viral infections. This protein, part of a protein family that has existed for hundreds of millions of years, has been one focus of Barr’s research.
Barr’s team discovered that HERC5 combats HIV in two primary ways: by trapping the virus’s genetic material within the cell nucleus, thus inhibiting its ability to replicate, and by altering HIV proteins to render them ineffective.
Role of unusual DNA structures
Barr’s current research delves into how HIV uses a unique method to integrate into our DNA.
“Our team identified non-canonical B-form DNA (non-B DNA) as a key player in this process. Unlike the well-known double helix structure of DNA, non-B DNA adopts various shapes and forms, creating patterns akin to a genetic form of Braille. HIV ‘reads’ these patterns to find suitable sites within the genome for replication or to remain dormant, evading current therapies,” explained Barr.
This finding highlights the complexity of HIV’s survival strategies and opens up new avenues for therapeutic intervention. Understanding these integration mechanisms could lead to treatments that either silence HIV expression in infected individuals or reactivate and destroy latent virus reservoirs, a major goal in curing HIV/AIDS.
Exploring HIV’s hideouts in the human body
Barr and his lab are currently extending their research to explore the hiding spots of HIV in different tissues, including the brain, esophagus, stomach, duodenum, and colon. This research is critical, as it sheds light on the virus's behavior in various parts of the body, not just the blood.
“We have discovered that HIV prefers specific regions in the genome, consistent across different individuals and tissues. Some of these favored spots are associated with genes linked to HIV-related diseases, suggesting a possible connection between the virus's integration points and the onset of these illnesses.”
The future direction of the Barr Lab is to unravel the precise mechanisms by which HIV targets non-B DNA. The goal is to develop innovative drugs that target these non-B DNA features. Such drugs could either permanently silence HIV or reactivate a larger fraction of the virus, making it susceptible to current cure strategies.









