SJHC Based Services
St. Joseph's Operational Stress Injury (OSI) Clinic
Located at the at Parkwood Institute, the St. Joseph’s Operational Stress Injury (OSI) Clinic is part of a national network of ten outpatient clinics funded by Veterans Affairs Canada to provide specialized mental health services to Veterans (and their family), members of the Canadian Forces, and the Royal Canadian Mounted Police (RCMP) with service-related psychological/psychiatric illness. St. Joseph’s OSI Clinic has two satellite clinics located in Toronto and Hamilton. Together, St. Joseph’s OSI Clinic provides service across Ontario including all Southwest Ontario, the Greater Toronto Area (GTA), Hamilton and Niagara region, and portions of Northern and Western Ontario.
The OSI clinic follows a standardized assessment and treatment protocol, including evidence-based psychotherapy and psychiatric care based on clinical practice PTSD guidelines developed by the Canadian Psychiatric Association, the Australian Centre for Posttraumatic Mental Health, the US DVA/DoD and the American Psychiatric Association. The specialized team of psychiatrists, psychologists, nurse practitioners, mental health nurses, and social workers provides comprehensive assessment and treatment in collaboration with community providers. St. Joseph’s OSI clinic has adopted an electronic treatment outcome monitoring system to further enhance treatment outcomes.
Embedded within a clinical and academic centre, the clinic provides training opportunities for learners, medical students, and residents. Community education, outreach, and research are also part of the OSI mandate. Currently there is a combined total of eight psychiatrists (part-time and full-time) working at our St. Joseph’s OSI sites in London, Hamilton and Toronto, all affiliated with the Department of Psychiatry, working predominantly with younger veterans with a geriatric psychiatrist providing psychiatric services for our older veterans population.
Medical Director, Dr. J. Don Richardson states, “St. Joseph’s OSI clinic will continue to strive to improve services and promote research in posttraumatic stress disorder and other operational stress injuries. With the current pandemic our goal is to enhance virtual care to our patients in the community through the Ontario Telemedicine Network (OTN) and other approved formats, improve outreach services to the GTA, Hamilton and Niagara region and further develop training opportunity for residents and psychiatrists interested in veterans’ mental health.”
Collaborative Mental Health Care Services
Overview
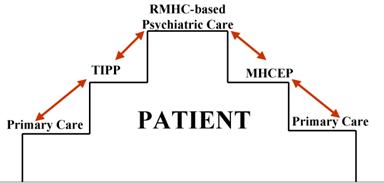
A psychiatric consultation team that visits a primary care practice on a regular basis to see and discuss patients, and to provide educational input and advice for primary care providers, has the potential to increase accessibility to psychiatric consultation, strengthen the support for primary care providers, and improve communication between psychiatrists and primary care providers. Such a program is expected to benefit the evolving Southwest Ontario mental health system by enhancing continuity of care, increasing accessibility to mental health services and promoting more efficient use of mental health services, which in other jurisdictions has led to a 46% reduction in the number of cases referred by participating physicians to outpatient services.
Learn more about Collaborative Mental Health Care
Regional Mental Health Care London (RMHCL) Collaborative Mental Health Care Services
“Stepping up services” and “stepping down services” comprise the two arms of the formal collaborative (shared) mental health care services that have been developed with identified treatment and support providers. Services include treatment, rehabilitation and support interventions to approximately 600 outpatients. RMHC London’s step-up service is named “Mental Health Consultation and Evaluation in Primary-care” (MHCEP). The step-down service is named “Transition into Primary-care Psychiatry” (TIPP). Consistent with a best practices model, program evaluation is an essential component of the MHCEP and TIPP operations. The MHCEP and TIPP program evaluation methodologies were approved by the University of Western Ontario Ethics Review Board.
Contact Us:
| Physician Clinical Team Leader: Dr. Jatinder Takhar, MD, FRCP(C) Collaborative Mental Health Care Services (MHCEP & TIPP) Professor Department of Psychiatry, Western University Phone: 519.455.5110, x.47185 Fax: 519.455.5679 |
Email: Jatinder.Takhar@sjhc.london.on.ca Address: Mood and Anxiety Program, St. Joseph’s Health Care London PO Box 5777, STN B London, ON N6A 4V2 |
Transition into Primary-care Psychiatry (TIPP)
TIPP, our “stepping down” service, provides transitional treatment and support for clients who are recovering from episodic or other types of mental health services and who are transitioning their care from ambulatory care to care by the primary care physician. The TIPP client base consists of Ambulatory Care clients and Prevention and Early Intervention Program for Psychoses PEPP clients who have maintained a sustained period of wellness and recovery as demonstrated by no significant medication adjustment or need for hospital based care over the last year.
TIPP Description of Service
The TIPP program is based on a modified version of Australia’s Consultation and Liaison in Primary-care Psychiatry (CLIPP) model.
Clients with stable but chronic mental illnesses will be transitioned back to the family physician with assistance from a team consisting of a psychiatrist and a nurse with mental health experience. Other services in the community may be utilized from time to time, according to client need. The model allows for on-site communication between primary care, psychiatry and the client in a least restrictive means with low stigma experience.
The program is unique in that it changes the culture of primary care practice and the balance of power among the team members. Essentially, the model serves as a concept for collaboration between professionals from all fields of health. The TIPP partners include community family physicians, London Health Sciences Centre, Canadian Mental Health Association (CMHA) - London, Western Ontario Therapeutic Communities Hostels (WOTCH), Choice and Opportunities in Rehabilitation and Education (CORE), Middlesex-London Health Unit, London Mental Health Crisis Service, London East Community Mental Health Centre, Telehealth Ontario and other specialty services.